In December 2019, reports of a mysterious outbreak of pneumonia-like cases in Wuhan, China emerged. In 2020, we watched Steven Soderbergh’s 2011 film “Contagion” become an eerie reality as countries entered national lockdowns and as biotech companies raced for a vaccine to the virus identified as SARS-CoV-2 or COVID-19. Currently, three vaccines have been given authorization for emergency use by the U.S. Food and Drug Administration (FDA) which include those developed by Pfizer-BioNTech, Moderna, and Johnson & Johnson. While these vaccines have restored a semblance of normalcy in the US, their efficacy against the variants and their duration of protection are still uncertain. Additionally, vaccine hesitancy has become a major concern in this pandemic despite their increasing accessibility. How else can we equip our body’s defenses against COVID-19?
New light is being shed on the development of antiviral drugs to prevent the spread of COVID-19 infection. Last month, the Department of Health and Human Services announced a $3.2 billion program to fund this area of research. Initially developed to treat Ebola virus, Veklury (remdesivir) is currently the only FDA-approved antiviral drug for treatment of COVID-19. The drug works by targeting the virus’s RNA-dependent RNA polymerase, inhibiting viral transcription and replication. However, the drug must be administered via infusion and its use is limited to circumstances of hospitalization. A virus’s main protease enzyme is another popular target of these antiviral drugs. Protease inhibitors are widely employed in the treatment of HIV/AIDS and Hepatitis C to slow disease progression. In March, Pfizer announced that it would begin Phase 1 trials of an oral antiviral pill after in-vitro studies demonstrated potent inhibition of the SARS-CoV-2 main protease.
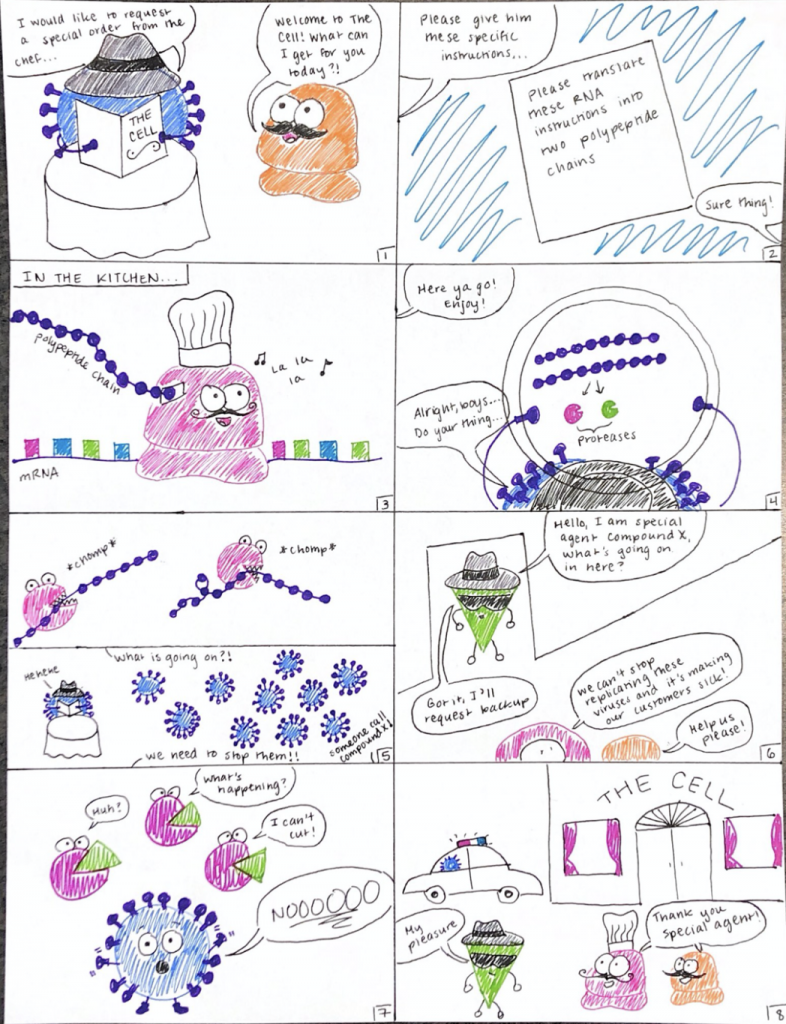
HOW DO PROTEASE INHIBITORS WORK?
Before we can understand the mechanism by which COVID-19 protease inhibitors might work, we need to break down the early stages of the virus’s life cycle.
All viruses lack the cellular machinery necessary to reproduce and must hijack host cells to execute this process. COVID-19’s unique structure allows for its attachment and entry into host cells. Its structure is a single strand of RNA enclosed in a special coating for proteins called a capsid.
Inside the host cell, the virus releases the RNA which contains the genetic instructions for the synthesis of two long polypeptides or protein chains. I breakdown the process of RNA translation into a polypeptide in this blog post. Two proteases, enzymes that cleave peptide bonds, are assembled from chunks of the larger polypeptide chains during this step. One of these proteases is the main COVID-19 protease.
In a normally functioning COVID-19 life cycle, the larger polypeptide chain gets cut up into smaller pieces by the proteases. These smaller pieces then get assembled by ribosomes of the host cell into other enzymes and machinery essential for the continuation of viral replication. However, protease inhibitors terminate this early step in the viral life cycle by binding tightly to the protease enzyme so that it can’t cut its targets. Without this critical function, the virus cannot replicate, preventing further infection.
MY RESEARCH
This summer, I had evaluated four compounds in a series of inhibition experiments of the main COVID-19 protease. It was an interesting change of pace from other experiments I have performed in the Pollock lab. You can find the pre-print for our paper that includes the biochemical inhibition assays and a ton of computational analyses by Justin Airas and Prof. Carol Parish here.
As the COVID-19 virus continues to mutate and new, more infectious strains emerge we need to expand our body’s arsenal of immune defenses. The development of oral therapeutic drugs that target the virus’ main protease is critical for early termination of viral replication. The technology could also be adapted for future viruses, not just COVID-19 and its variants, as many viruses rely on this enzyme. The key difference between vaccines and antiviral drugs is that vaccines prevent or mitigate infection, while antiviral drugs are used to treat individuals already infected by a virus. When prescribed early, oral antiviral drugs could still offer protection for unvaccinated individuals and mitigate worsening symptoms.

Wonderful work!