“Any chronic medical condition that defies diagnosis should be regarded as celiac disease until proven otherwise” –Dr. John Weiner, Australian Allergist
We established in Part 2 of the series that celiac disease wreaks some pretty serious havoc on your gut; but what happens with non-celiac gluten intolerance? What is it?
Well these questions are the key mysteries that led to the inception of this project.
Non-celiac gluten intolerance (NCGI) is not the easiest thing to diagnose as there are no known biological mechanisms to define it.
Celiac Disease and wheat allergies can be detected through blood testing (fancily named: serology) to determine presence of antibodies, as discussed in Part 2.
In NCGI patients research has yet to show a significant presence of these antibodies even after a gluten challenge.
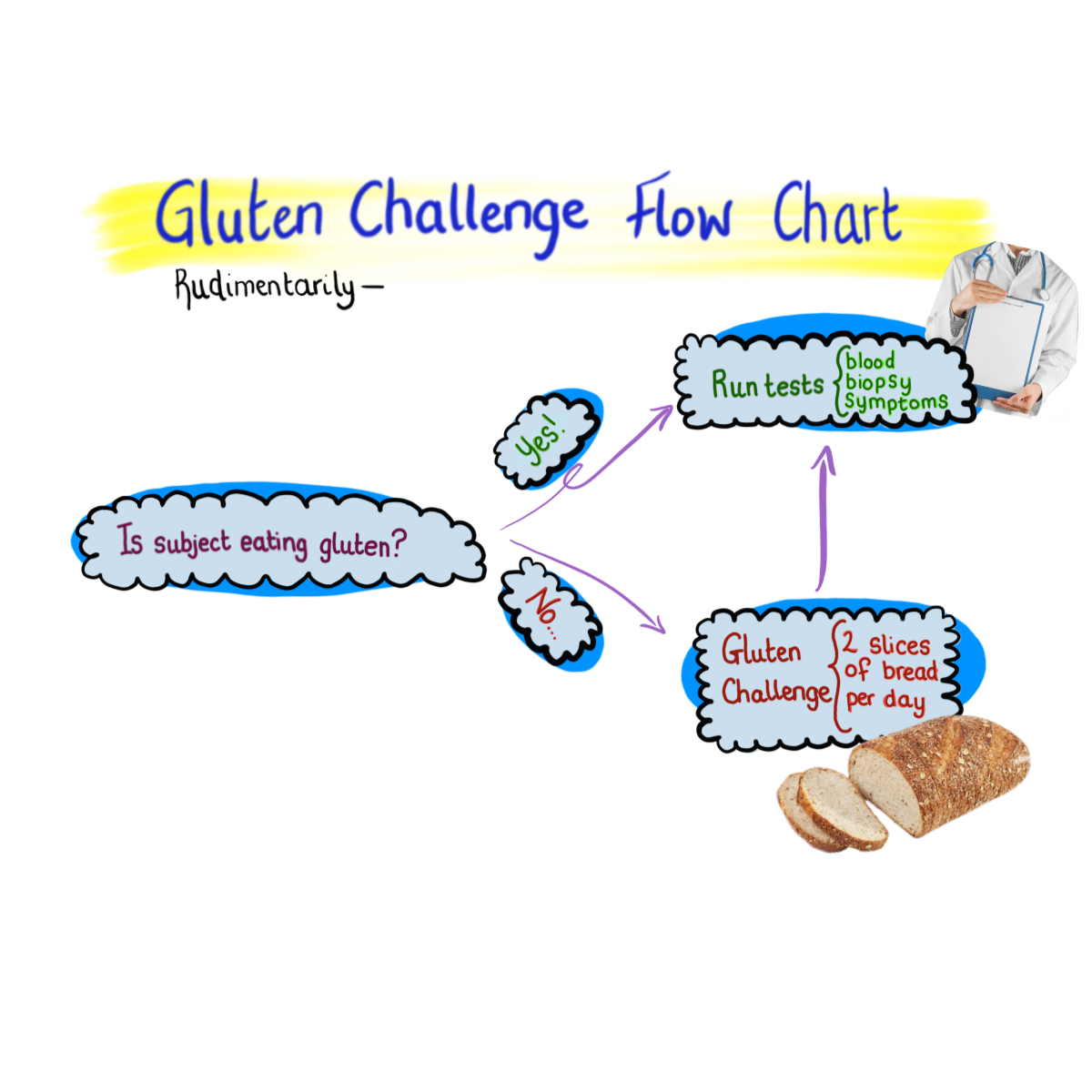
A gluten challenge (as illustrated above) the patient needs to be challenged by gluten for a standard amount of time, usually 2-6 weeks, in order to run appropriate testing to detect antibodies or inflammation that is gluten induced. This is utilized if the patient has been adhering to a Gluten-Free diet before consulting.
NCGI is often characterized by key extra intestinal and intestinal symptoms. These include foggy brain, abdominal pain, poor digestion, diarrhea or constipation (sometimes both!) and rash.
As you may imagine, if eating gluten causes severe discomfort, this method is not the most desirable process so many forego an official diagnosis.
However, many studies show that after gluten challenges many NCGI patients continue to have symptoms and significantly so. Even images taken of the small intestine fail to show the large amount of IEL (police), villous atrophy, or inflammation that has become a defining characteristic in the leading gluten intolerant disorder, celiac disease.
Yet, some reviews have gone on to invalidate prior controlled studies, indicating that the amount of gluten was not controlled and people with NCGI could have other undiagnosed conditions.
Notably, NCGI is a condition known only to improve with the withdrawal of something, whereas other intolerances and conditions can often be described by what’s lacking in our natural bodies.
For example, if someone has a lactose intolerance, their body lacks lactase, the enzyme responsible for breaking lactose down. There may be a mechanism that describes the nebulous NCGI condition, but research remains in an argumentative (ahem* cough* I mean, discussion stage). More on that in Part 4.
Newer studies that analyze the gluten challenge trial have gone further to control it, making sure that participants and experimenters are blind to condition. These experiments often show significant severity of symptoms, compared to a placebo. However, no change in the biological markers.
Most notably, a recent exploration with 59 adults by Skodje and colleagues at the K. G. Jebsen Celiac Disease Research Centre, found that after people ingested bars of fructan, gluten or placebo. The fructan bar was the most symptom inducing among those that are reportedly gluten sensitive.
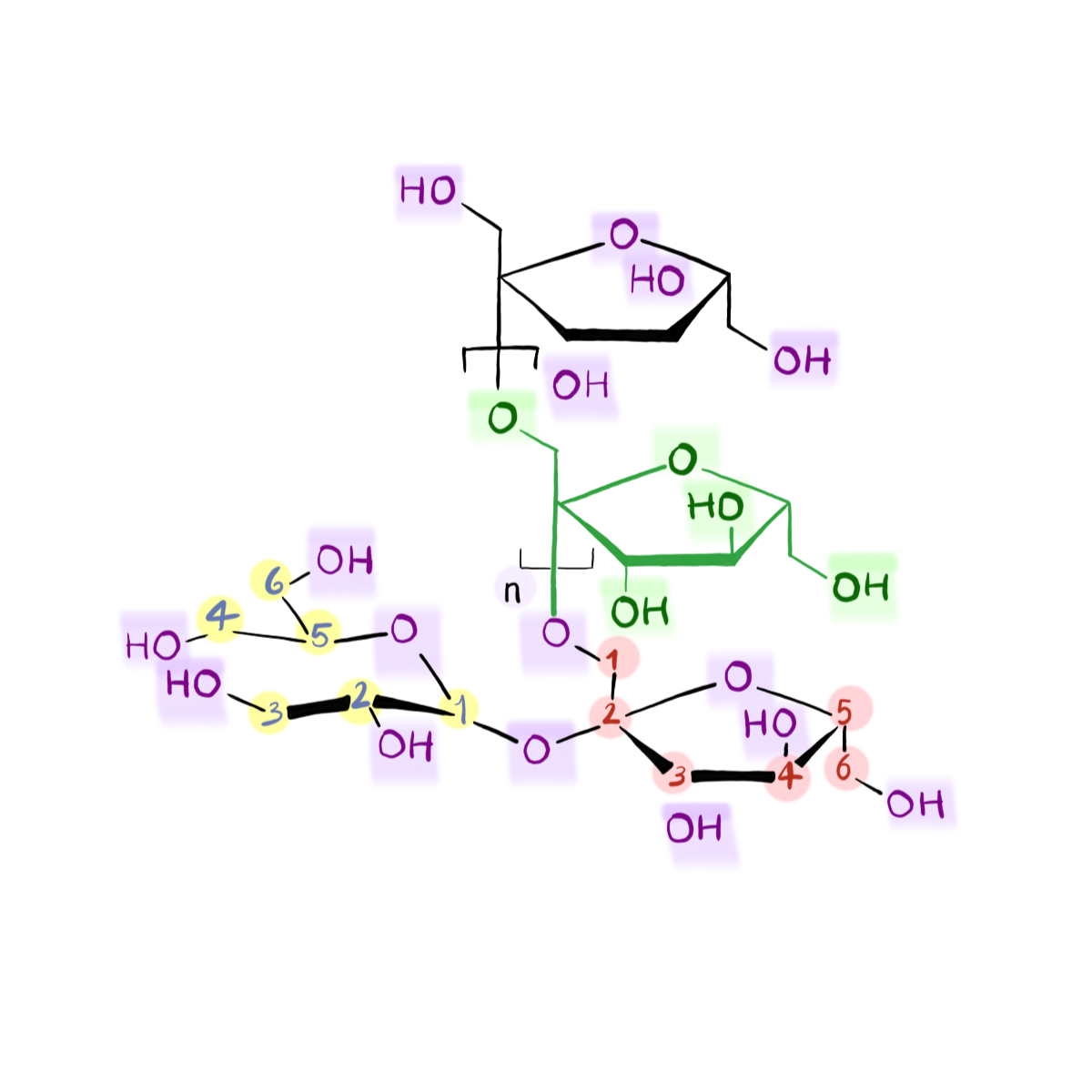
So could fructan be the new culprit? The next molecule to blame digestion and poor health on, let’s talk on Friday!