In Part 3, I discussed how recent research suggests fructans have a bigger role in non-celiac gluten intolerance, and possibly could replace gluten as the main offender. Let’s start with them.
Fructans, which are sugars composed of fructosyl units (don’t worry too much about what that is), are found in a multitude of foods such as wheat, rye, onions, artichokes, brussel sprouts, watermelon, and cashews. Quite the array.

The scientific basis for their problematic nature is quite sound. They are part of a group called FODMAPs, and if you’re familiar with any dietary restrictions for intestinal or irritable bowel syndrome, a low FODMAP diet is the standard recommendation.
This isn’t ideal as FODMAPs (which stands for Fermentable Oligo-, Di-, Mono-sacchardies and Polyols) encompass a lot of foods. Therefore, the diet is usually a last resort, especially since the “F”, or “fermentable”, property of the food group is a healthy normal process for your gut.
FODMAPs undergo these fermentation processes in your large intestine because they are not naturally digested by your body. The gas production from fermentation can cause bloating and expansion of the intestine that is uncomfortable and sometimes the source of bad digestive symptoms for those that are more sensitive to FODMAPs.
Yet in the case of non-celiac, that foggy brain, headache, rash or fatigue feeling would not be a probable result of FODMAPs. Since fructans and other FODMAPs ferment in the gut, they can have an impact intestinally but rarely have an extra-intestinal impact. The extraintestinal impact, which includes symptoms outside the digestive tract, has come to be the primary marker with non-celiac gluten intolerant patients.
Although fructans can cause discomfort, they may not be the sole source of particularly evasive NCGI cases.
Another likely possibility is amylase trypsin inhibitors, or ATIs.
ATIs are the bodyguard of the grain. They are responsible for protecting the plant from getting digested when it is growing. In nature, this means protection from pests.
Trypsin, from part 1, is an enzyme in the intestine that breaks down proteins, like gluten. As the name suggests, an ATI, or amylase trypsin inhibitor blocks trypsin function. In the fashion of a good bodyguard, ATIs continuously block trypsin’s attempts to digest proteins, making it harder and harder to break food down when more ATIs are present.
Wheat that contains more ATIs is known to have higher yields and greater pest resistance. A sensible correlation since no one wants to mess with wheat that has a bunch of bodyguards.
However, humans are much much larger than a dingy little enzyme. Therefore, when we pluck wheat to eat it and ATIs enter our system, they are still trying to protect gluten and the nutrients within the endosperm as much as possible.
Indeed it is an interesting culprit. In a country like the United States where wheat is grown abundantly, specifically for its pest resistance and high yields, these abundant ATI strains are surviving again and again.
A comparison of the amount of ATIs in modern wheat compared to “old” wheat has been suggested in editorials, but yet to be completed. This may explain the increase in prevalence of gluten-free eating and especially more milder cases.

The final culprit I’ll evaluate, which is not often researched as it pertains to non celiac gluten intolerant individuals, is histamine intolerance. There are many claims, but little experimentation on how NCGI might be explained by an intolerance normally untested for. Previously this has meant fructose, FODMAPs, lactose. But researchers within the European Histamine Research Society offer up a common target for inflammation: histamine intolerance.
Histamine? Isn’t that the thing that has anti- in front of it on my allergy medications??
Haha yes. That one.
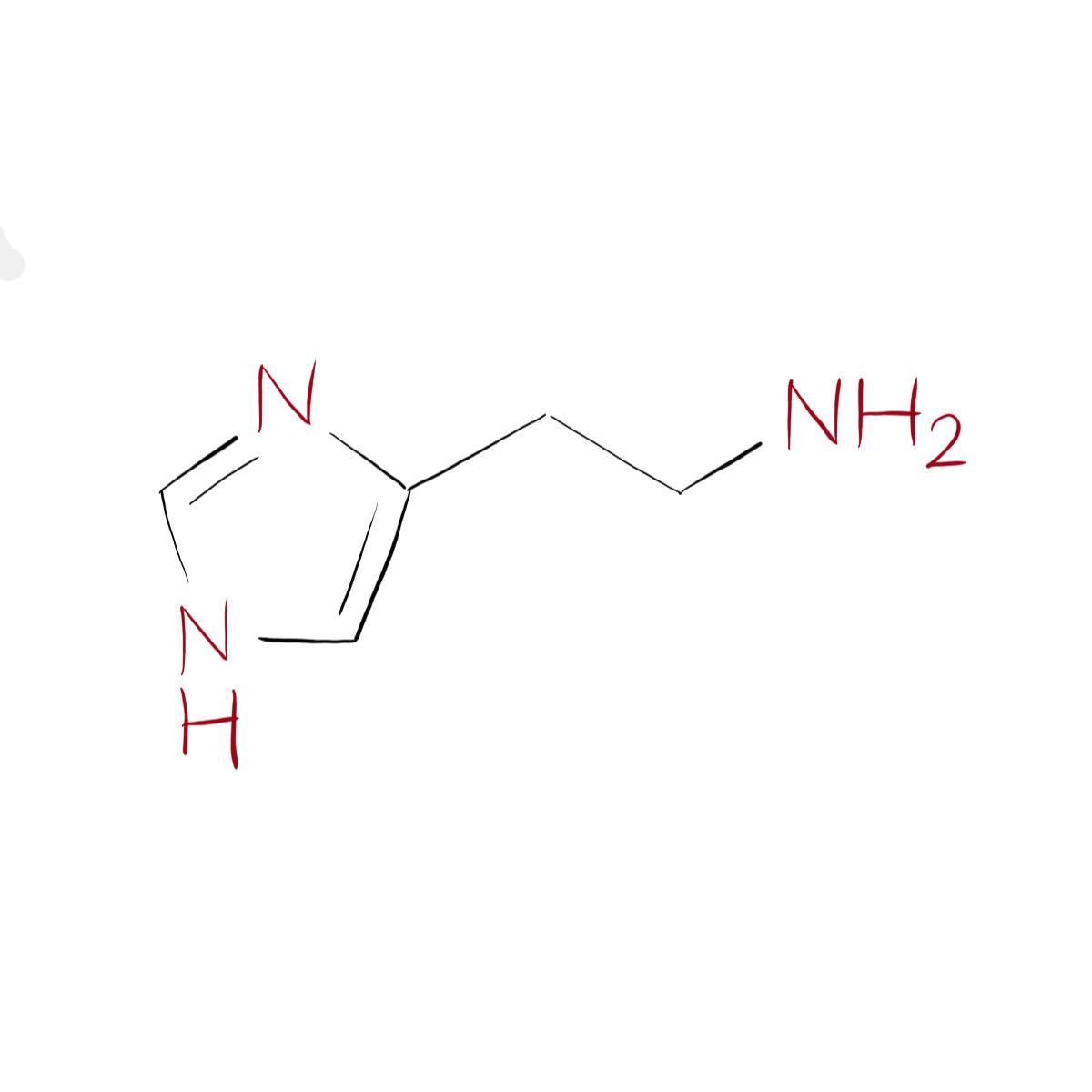
It is a biogenic amine (structure pictured above) that can be digested from foods or be changed from histidine; a naturally occuring amino acid in your body.
High histamine foods are tomatoes, beans, cheese, alcohol, chocolate, ham, salami, and sausage. It is not found in yeast, but yeast can speed up the process of histidine turning into histamine, meaning yeast containing products (that usually have gluten), or high histamine foods (that are usually served alongside gluten) may have gone unnoticed.
Histamine is also quite variable in content. Depending on maturation process, fermentation, processing, or ripeness, the amount of histamine content may vary, explaining why certain foods may be more troublesome from one day to the next.
In the body, histamine is quite a nosy molecule. Like a pesky sibling it can affect many of your bodily systems and can mess other things up-like turning histidine into histamine.
Histamine is processed in your gut within the mucosal layers described in part 2 and when digested, is mostly processed by Diamine Oxidase, or DAO.
Histamine intolerance is an imbalance of DAO and histamine. Naturally, our DAO levels can break down the amount of histamine typically present or ingested. With reduced levels of DAO, histamine can not be broken down and it builds up. The build up can cause symptoms such as headaches, poor digestion, and fatigue (sound familiar?)
And the kicker. People that have common GI ailments are often found to have low DAO levels. When NCGI patients have been tested for DAO activity, it was reduced compared to normal.
Although the case for histamine is enticing and lines up quite strongly, targeted research on histamine and gluten is still needed.
Unfortunately, this means that a decisive end to NCGI was not going to be magically revealed within this part. Regardless, I hope this four part look into a pervasive phenomenon has left you more informed and excited to become scientifically informed! Although, a magical reveal would be fantastic.
Accompanying art for this article created by Molly Yon Hin